It’s not even the reporting tool for which your clinicians have been asking!
I have attended between four and eight patient safety and quality healthcare conferences a year for the past five years. Personally, I enjoy the opportunities to learn from what others are doing in the space. My expertise lies at the intersection of quality and technology; therefore, it’s what I’m eager to discuss at these events. I am most interested in understanding how health systems are addressing the burgeoning financial burden of reporting more (both internal and external compliance and regulatory mandates) with less (from tightening budgets and, quite honestly, allocating resources to the wrong places for the wrong reasons).
 Let me be frank: there is job security in health care analysts, “report writers,” and decision support staff. They continue to plug away at reports, churn out dated spreadsheets, and present static, stale data without context or much value to the decision makers they serve. In my opinion, patient safety and quality departments are the worst culprits of this waste and inefficiency.
Let me be frank: there is job security in health care analysts, “report writers,” and decision support staff. They continue to plug away at reports, churn out dated spreadsheets, and present static, stale data without context or much value to the decision makers they serve. In my opinion, patient safety and quality departments are the worst culprits of this waste and inefficiency.
When I walk around these conferences and ask people, “How are you reporting your quality measures across the litany of applications, vendors, and care settings at your institution?,” you want to know the most frequent answer I get? “Oh, we have Epic (Clarity)”, “Oh, we have McKesson (HBI),” or “Oh, we have a decision support staff that does that”. I literally have to hold back a combination of emotions – amusement (because I’m so frustrated) and frustration (because all I can do is laugh). I’ll poke holes in just one example: If you have Epic and use Clarity to report here is what you have to look forward to straight from the mouth of a former Epic technical consultant:
“It is impossible to use Epic “out of the box” because the tables in Clarity must be joined together to present meaningful data. That may mean (probably will mean) a significant runtime burden because of the processing required. Unless you defer this burden to an overnight process (ETL) the end users will experience significant wait times as their report proceeds to execute these joins. Further, they will wait every time the report runs. Bear in mind that this applies to all of the reports that Epic provides. All of them are based directly on Clarity. Clarity is not a data warehouse. It is merely a relational version of the Chronicles data structures, and as such, is tied closely to the Chronicles architecture rather than a reporting structure. Report customers require de-normalized data marts for simplicity, and you need star schema behind them for performance and code re-use.”

You can’t pretend something is what it isn’t.
Translation that healthcare people will understand: Clarity only reports data in Epic. Clarity is not the best solution for providing users with fast query and report responses. There are better solutions (data marts) that provide faster reporting and allow for integration across systems. Patient safety and quality people know that you need to get data out of more than just your EMR to report quality measures. So why do so many of you think an EMR reporting tool is your answer?
There is a growing sense of urgency at the highest levels in large health systems to start holding quality departments accountable for the operational dollars they continue to waste on non-value added data crunching, report creation, and spreadsheets. Don’t believe me? Ask yourself, “Does my quality team spend more time collecting data and creating reports/spreadsheets or interacting with the organization to improve quality and, consequently, the data?”
Be honest with yourself. The ratio, at best, is 70% of an FTE is collection, 30% is analysis and action. So – get your people out of the basement, out from behind their computer screens, and put them to work. And by work, I mean acting on data and improving quality, not just reporting it.






 specialties; or you the “behemoth”, the one with the health plan, physician group, outpatient, inpatient, and multi-discipline, multi-care setting institution. Is your EMR really just an electronic filing cabinet? Do nursing and physician notes, standard lab and imaging orders, registration and other critical documents just get scanned into a central system that can’t be referenced later on to meet your analytic needs? Don’t worry, you’re not alone…
specialties; or you the “behemoth”, the one with the health plan, physician group, outpatient, inpatient, and multi-discipline, multi-care setting institution. Is your EMR really just an electronic filing cabinet? Do nursing and physician notes, standard lab and imaging orders, registration and other critical documents just get scanned into a central system that can’t be referenced later on to meet your analytic needs? Don’t worry, you’re not alone… standard ontology for displaying and navigating the unstructured information collected by providers across care settings and patient visits (see
standard ontology for displaying and navigating the unstructured information collected by providers across care settings and patient visits (see 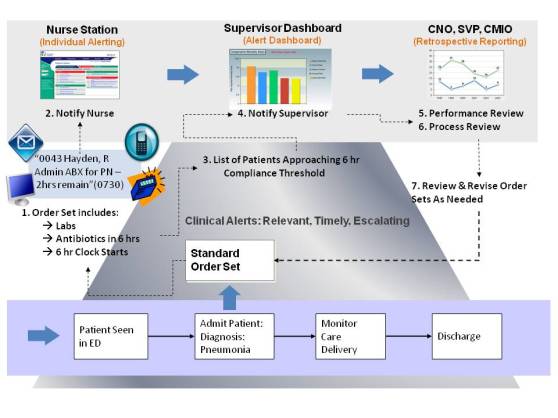
 Why is the concept of No Data Left Behind important? Clinicians have stated emphatically, “we do not know what questions we’ll be expected to answer in 3-5 years, either based on new quality initiatives or regulatory compliance, and therefore we’d like all the raw and unfiltered data we can get.” Additionally, the recent popularity of using clinical dashboards and alerts (or “
Why is the concept of No Data Left Behind important? Clinicians have stated emphatically, “we do not know what questions we’ll be expected to answer in 3-5 years, either based on new quality initiatives or regulatory compliance, and therefore we’d like all the raw and unfiltered data we can get.” Additionally, the recent popularity of using clinical dashboards and alerts (or “ Providers must formulate a strategy to capitalize on the mountains of data that will come once the healthcare industry figures out how to
Providers must formulate a strategy to capitalize on the mountains of data that will come once the healthcare industry figures out how to